Prostate Cancer Resources for Patients
Tools
Educational Materials
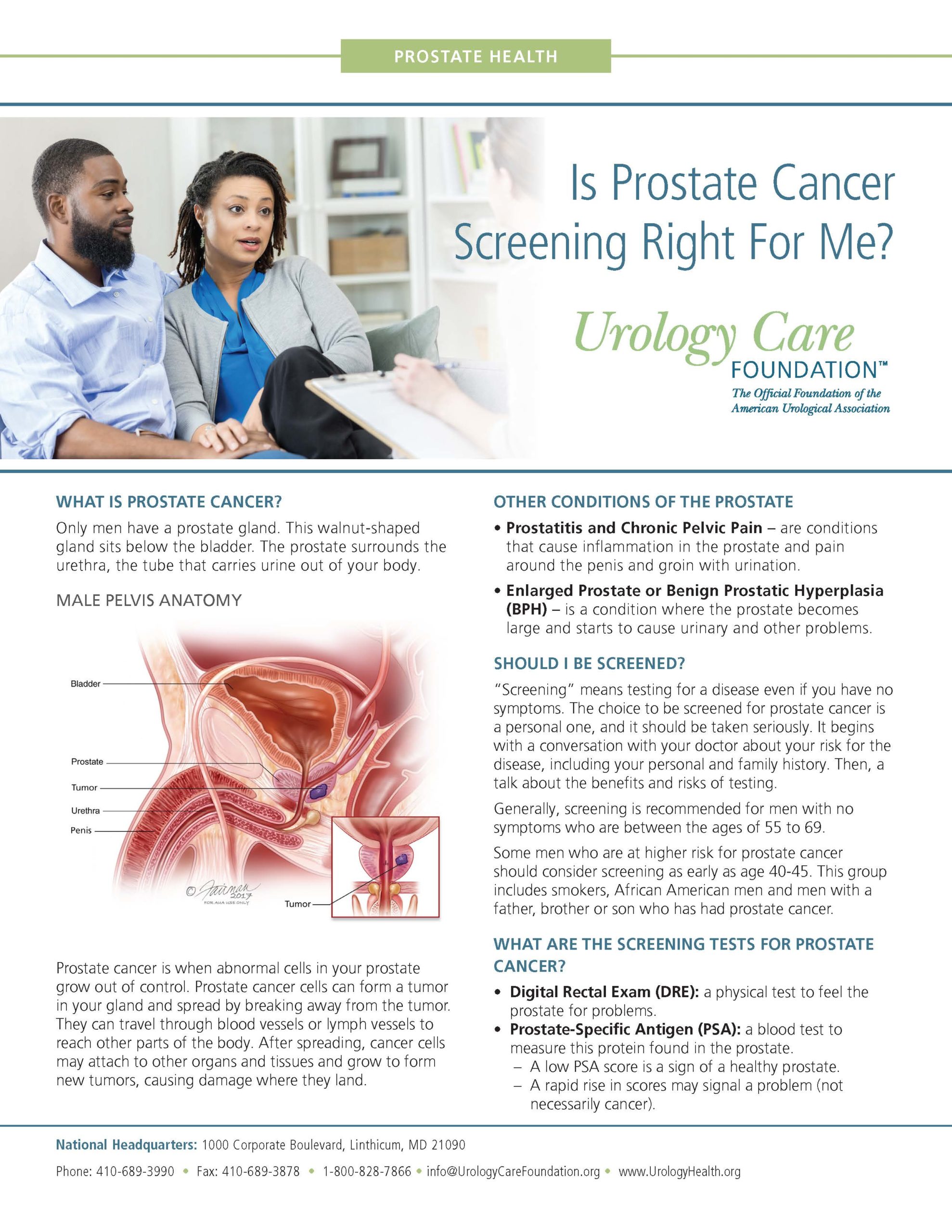
The prostate is roughly the size of a walnut and sits right below the bladder, surrounding the urethra which is the tube that carries urine from the bladder out through the penis. The prostate and seminal vesicles (two, smaller paired glands attached to each side of the prostate) are part of the male reproductive system and their main job is to make fluid for semen.
Content within askMUSIC is provided by the Urology Care Foundation.
If prostate cells grow abnormally, they can form a tumor, in the prostate gland. Tumors can be either benign (non-cancerous) or malignant (cancerous). Prostate cancer cells can remain inside the prostate gland or they can travel and invade nearby tissues.
Even if you are diagnosed with prostate cancer, many men will not die from it, but rather from other causes. Most prostate cancer is slow growing and many are cured after having treatment.
Though it is not known how or why prostate cancer starts, many factors may increase risk for the disease. Some of these include:
In the early stages, prostate cancer often has no symptoms. When symptoms do occur, they can be like those of an enlarged prostate called benign prostatic hyperplasia (BPH). Prostate cancer can also cause symptoms unrelated to BPH. If you have urinary problems, talk with your healthcare provider about them.
Symptoms of prostate cancer may include the following:
-
-
- Dull pain in the lower pelvic area
- Frequent urination and/or trouble urinating (pain, burning, or weak flow)
- Blood in the urine
- Painful ejaculation
- Pain the lower back, hips or upper thighs
- Loss of appetite and/or weight
- Bone pain
-
Content within askMUSIC is provided by the Urology Care Foundation.
Screening for prostate cancer refers to testing for the disease through two ways: prostate-specific antigen (PSA) blood test and digital rectal examination (usually performed by a doctor in the exam room). These are not perfect, and abnormal tests from either test may be due to an enlarged cancer, not cancer. Even if you don’t have symptoms, it’s important to screen for prostate cancer early.
Screening is recommended if you are a man and meet one of the following criteria:
- Between 55-69 years old
- African American and over 40 years old
- Have a family history of prostate cancer
This recommendation is from a guideline issued by the American Urological Association.
For a short video on if prostate cancer screening is right for you, please see below:
What is the prostate-specific antigen, or PSA, blood test?
PSA is a blood test measuring the amount of prostate-specific protein being produced by the prostate. PSA is produced in the prostate. Checking your PSA levels may help detect prostate cancer early.
For a short video on PSA testing, please see below:
What is a Digital Rectal Exam (DRE)?
A DRE is when a healthcare provider examines the prostate by placing a lubricated, gloved finger in the rectum. The doctor feels for an abnormal shape or thickness to the prostate.This test cannot detect early cancer by itself and should be done with a PSA test.
Content within askMUSIC is provided by the Urology Care Foundation.
In the early stages, prostate cancer often has no symptoms. When symptoms do occur, you may experience urinary symptoms, like those of an enlarged prostate called Benign Prostate Hyperplasia (BPH). Prostate cancer can also cause symptoms unrelated to BPH. If you have urinary problems, talk with your healthcare provider about them.
Symptoms of prostate cancer may include the following:
- Dull pain in the lower pelvic area
- Frequent urination and/or trouble urinating (pain, burning, or weak flow).
- Blood in the urine (hematuria)
- Painful ejaculation
- Pain in the lower back, hips or upper thighs
- Loss of appetite and/or weight
- Bone pain
Content within askMUSIC is provided by the Urology Care Foundation.
Prostate cancer is diagnosed by a prostate biopsy. During a prostate biopsy procedure, tiny pieces of tissue are removed from the prostate and examined under a microscope by a pathologist (a doctor who will look at the tissue specifically for cancer cells). A biopsy report is provided to your doctor which includes useful information to determine if there is cancer.
For a short video on what you should know about a prostate biopsy, please see below:
 What is the Gleason Score?
What is the Gleason Score?
After a prostate biopsy, a pathologist looks at your cells found within the tissue and compares abnormal cells to healthy cells. They assess how likely they are to grow and spread by assigning a Gleason Score to each tissue sample to decide the risk of the disease and to make an accurate diagnosis.
Gleason scores are recorded between 3 – 5 (3 having less abnormal cells or low risk cancer and 5 having a lot of abnormal cells or higher risk cancer). The two most common grades/patterns (known as primary and secondary pattern) found in the biopsy sample are then combined to a Gleason score. A Gleason Score is written as Pattern 1+ Pattern 2 = Overall Gleason Score, helping you and your doctor understand if the cancer is low, intermediate, or high risk.

What is staging?
Along with a Gleason score, the tumor is also staged and can be determined by a DRE and imaging (e.g., transrectal ultrasound) to describe where the cancer is within the prostate, hoe extensive it is, and if it has spread to other parts of the body. The system used for staging is called TNM staging which stands for Tumor, Nodes, and Metastasis.
- Tumor (T) Stage: Determined by biopsy or DRE results
- Nodes (N) Stage: Determined by CT Scan
- Metastasis (M) Stage: Determined by Bone Scan
Choice of Treatment for Prostate Cancer is Based on a Shared Decision Between You and Your Doctor
The choice of treatment for prostate cancer depends on factors related to the severity and extent of the cancer, as well as, your preferences related to the benefits and side effects of treatment. Talk to your doctor and your family as you consider what treatment option is best for you.
For a short video on prostate cancer treatment options testing, please see below.
Making a Shared Decision
To help newly diagnosed prostate cancer patients make an informed decision, with their doctor about their treatment options, your doctor may encourage you to participate in the MUSIC Personal Patient Profile-Prostate Program (P3P). MUSIC partnered with TrueNTH, a Movember Foundation project dedicated to improving the quality of care for prostate cancer patients. to bring the P3P tool to patients in Michigan. Patients complete a onetime online questionnaire answering questions regarding patient function and preferences. Then they are presented with tailored treatment and given general prostate cancer information to help patients and their doctor determine a treatment best suited for them.
If your urologist in Michigan enrolls you in the Personal Patient Profile-Prostate (or “P3P”), please access this tool via the direct e-mail invitation you received. If your doctor does not participate in the MUSIC P3P Program, you can click on the TRUE Nth logo to access the tool:
To learn more about the MUSIC P3P program, please click on the image below:
TRUENTH-MUSIC-P3P-Patient-Brochure-updated
Content within askMUSIC is provided by the Urology Care Foundation.
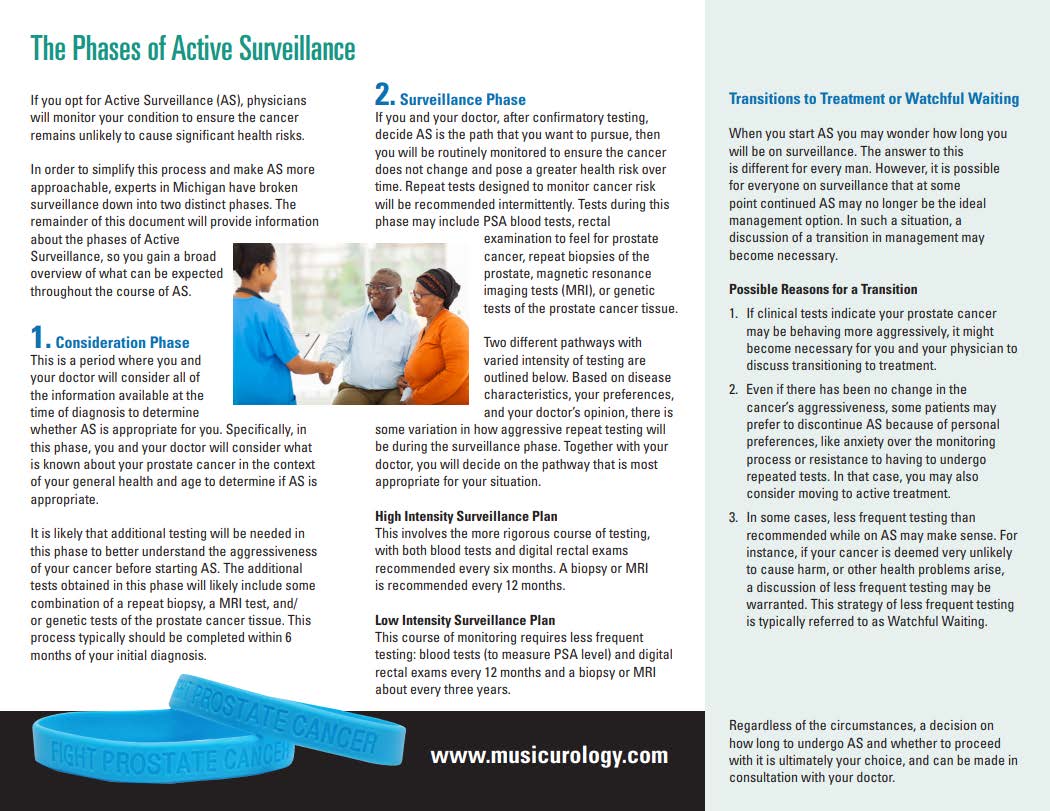
 Active Surveillance
Active Surveillance
Active Surveillance (AS): active monitoring of prostate cancer; scheduled follow-up visits every 6-12 months including PSA blood test, DRE, repeat biopsy or MRI imaging.
May be a good option for men who:
- have small, slow-growing, low-risk prostate cancer
- are older or those who have other serious medical conditions
To learn more about Active Surveillance for prostate cancer, please click on the image below:
Content within askMUSIC is provided by the Urology Care Foundation.
 Watchful Waiting
Watchful Waiting
Watchful Waiting (WW): less involved system of monitoring of prostate cancer. Follow-up tests include PSA blood test and DRE, and it does not require repeat biopsies or imaging tests.
May be a good option for men who:
- do not want treatment
- have other medical conditions that would interfere with active treatment

Content within askMUSIC is provided by the Urology Care Foundation.
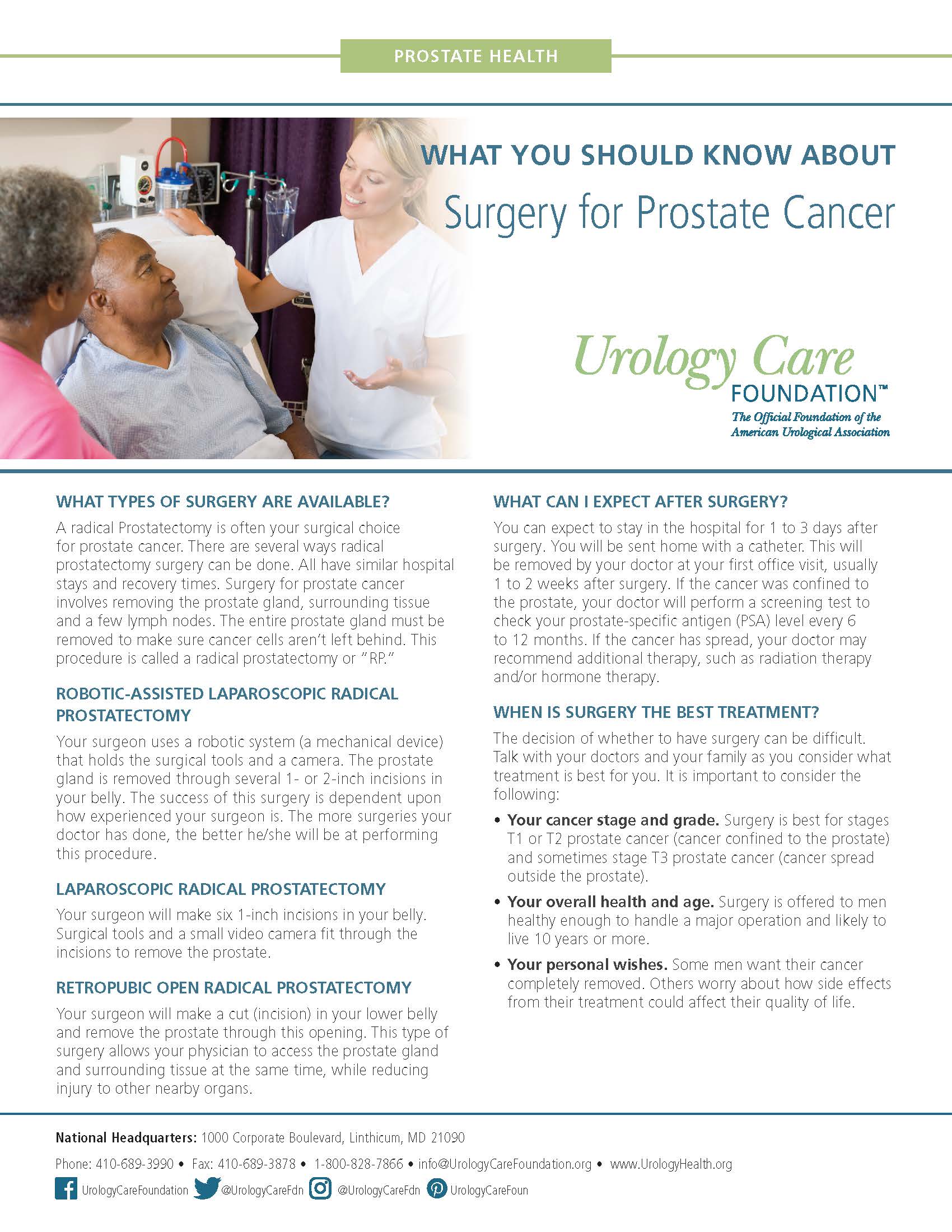
![]() Radical Prostatectomy
Radical Prostatectomy
Radical prostatectomy: surgery to remove the prostate from the body.
May be a good option for men who:
- have cancer stages T1, T2 (cancer confined to the prostate), and sometimes T3
- are healthy enough to handle a major operation
- have a personal preference to have the cancer completely removed
How will I feel if I have my prostate surgically removed?
Every patient’s journey is different, but some of the most common side effects are urinary leakage and erection problems.
To help your doctor understand your symptoms and optimize your recovery pathway, your doctor will encourage you to participate in the MUSIC Patient Reported Outcomes (PRO) program. As part of the PRO program, patients complete a questionnaire related to their health and function, before and at several time points after the surgery.
To learn more about the MUSIC PRO program, please click on the image below:
What does sexual recovery after prostate cancer surgery look like?
Although each patient’s postoperative journey is individual, sexuality is more than just having and maintaining erections. The TrueNTH Sexual Recovery Intervention is an online, tailored interactive program to support men and their partners on their journey toward sexual recovery after prostate cancer treatment. It was developed by funding from the Movember Foundation and is designed to help patients understand key points and provide ideas for how to work on sexual recovery alone or with a partner. Register to find out more about what you can do to address this common issue.
The TrueNTH Sexual Recovery Program can help in several ways:
- Supports couples in staying sexually connected before, during, and after prostate cancer treatment
- Encourages rehabilitation to improve sexual function
- Improves communication about sexual issues to promote satisfying sexual relationships
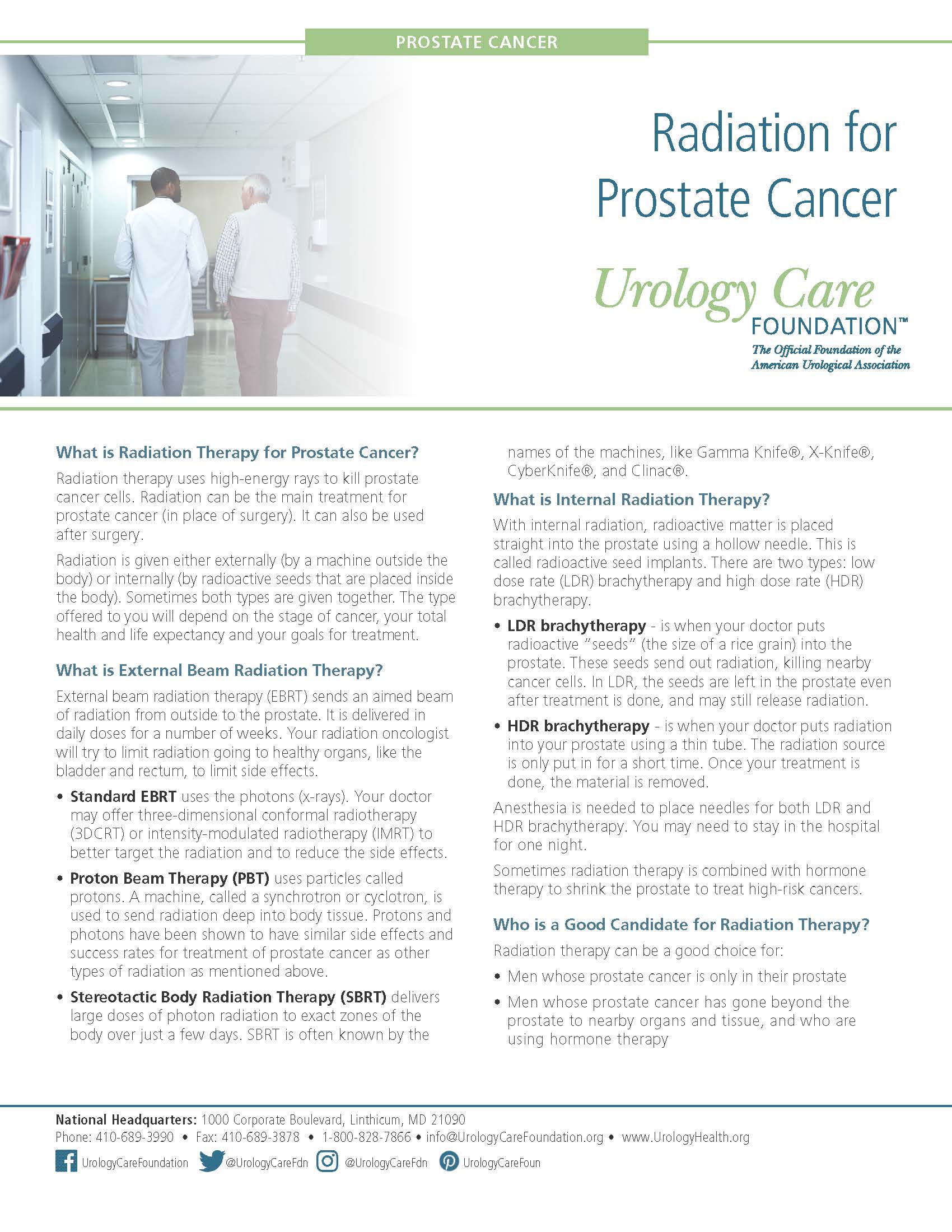
 Radiation Therapy
Radiation Therapy
Radiation therapy: uses high-energy beams to kill or slow the growth of cancer cells; may be used as a primary treatment or after surgery.
May be a good option for men:
- whose cancer is confined to the prostate
- whose cancer has gone outside of the produce and are using hormone therapy
- had their prostate removed but are at risk for the disease to come back
- have had prostate cancer come back
- have advanced prostate cancer
Content within askMUSIC is provided by the Urology Care Foundation.
 Chemotherapy
Chemotherapy
Chemotherapy: drug administered intravenously (through a vein) or by mouth to kill cancer cells.
May be a good option for men with:
- cancer that has spread outside of the prostate
- advanced prostate cancer stages or that no longer responds to hormone therapy
Most of these side effects can be managed, and lessen once treatment ends. To learn more about chemotherapy, click on the link below:
Download an informational document on chemotherapy
Content within askMUSIC is provided by the Urology Care Foundation.
![]()
Hormone Therapy:
Androgen deprivation therapy (ADT): uses drugs to block or lower testosterone as well as other male sex hormones that fuel cancer to grow.
May be a good option for men who:
- have prostate cancer that has returned after treatment
- have advanced prostate cancer
- are undergoing radiation treatment
Download an informational document on hormone therapy
Content within askMUSIC is provided by the Urology Care Foundation.
The following questions may be helpful to ask your doctor to better understand your diagnosis and available treatment options that are best suited for your prostate cancer care.
Diagnosis:
- What is my Gleason score, the grade and the stage of my cancer?
- How aggressive is this cancer? Is it likely that my cancer will spread? (Has it spread?)
- If the cancer has spread, where?
- Do I need more tests now?
- What type of schedule should I be on to track changes with this cancer?
Treatment:
- What are my treatment choices (including surveillance, localized therapy or systemic therapy)?
- What are the advantages and disadvantages of each?
- What are the time considerations and costs for each?
- What is your experience with each option?
- Would I have to go somewhere special to get treatment?
- Why do you recommend one type of therapy over another?
- What are the chances for each treatment to manage my cancer and for how long?
- What are the chances of complications from each treatment?
- What kinds of complications are likely from each?
- When are they likely to occur?
- What if I choose no treatment (watchful waiting or active surveillance)?
- How often will I need to take follow-up tests?
- If I use hormone therapy, what type do you suggest and why?
- How would we manage potential side effects from hormone therapy?
- What are the chances that my cancer will return after treatment – and if it does, what options for treatment do I have then?
- Can we develop a short and long-term plan for my care?
- Is there someone you would recommend for another opinion?
Side Effects & Recovery:
- What are the potential side effects of the treatment you recommend: both immediately and in the long term?
- How can I manage side effects?
- How would we manage potential urinary dysfunction and for how long?
- How would we manage potential erectile dysfunction and for how long?
- What other side effects should I consider?
- How much recovery time will be required after surgery?
- Will I need to take time off from work or other activities to manage treatment and treatment side effects?
Content within askMUSIC is provided by the Urology Care Foundation.
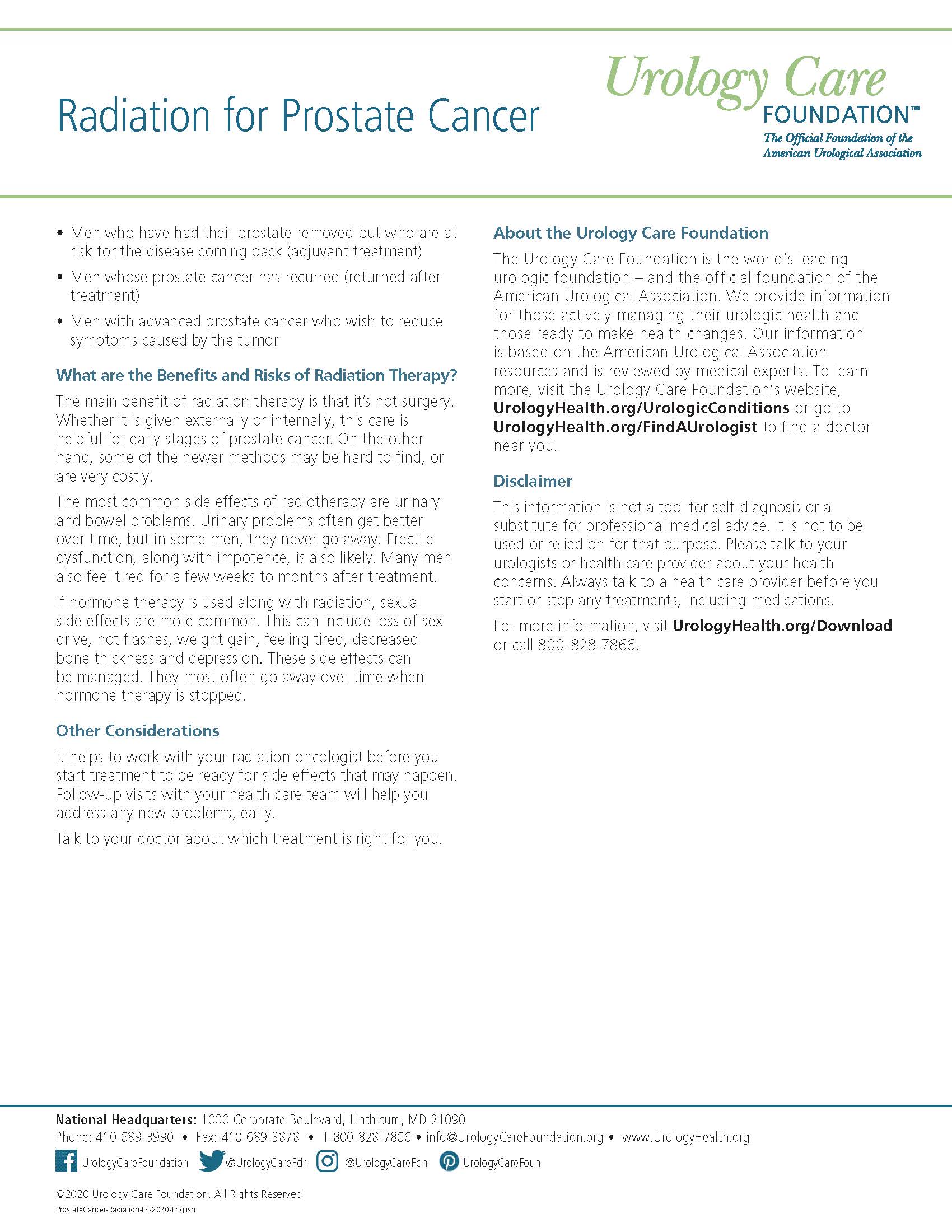
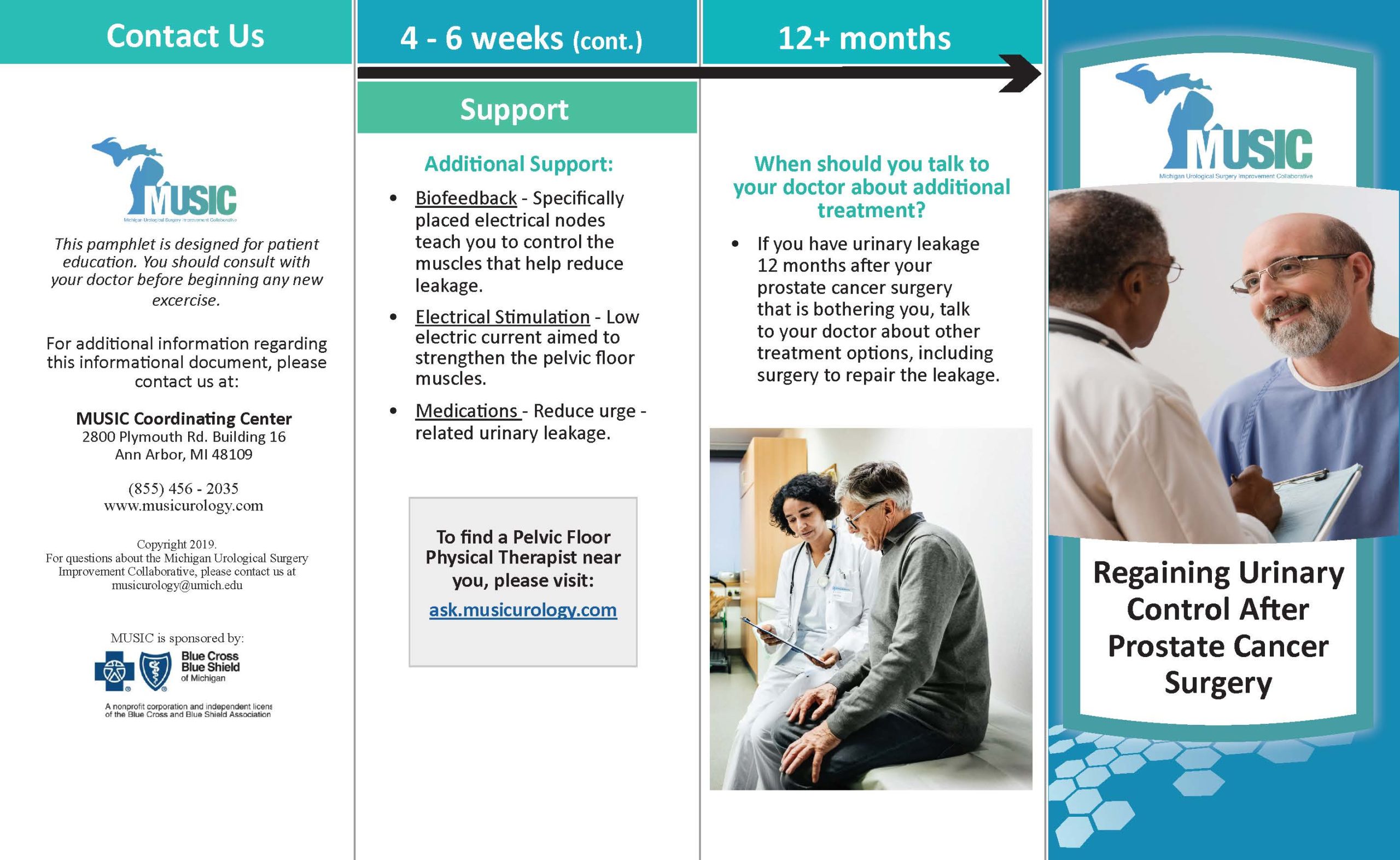
Kegel exercises help strengthen muscles, called pelvic floor muscles, that are involved with urinary control.
If you are pursuing surgery for your prostate cancer treatment, your doctor may have recommended you start doing Kegel exercises. Some doctors may suggest beginning Kegel exercises before while others may suggest beginning Kegel exercises after surgery. Please talk to your doctor about when to start your Kegel exercises.
Content within askMUSIC is provided by the Urology Care Foundation.
Finding a Pelvic Floor Therapist Near you
To find a pelvic floor physical therapist near you, please click on area closest to you below: Finding the right pelvic floor physical therapist should be a decision between you and your doctor. Your doctor may recommend a pelvic floor therapist not on this list. Please talk with your doctor to find out which pelvic floor physical therapist may be best for you and your care.
To learn more about Kegel exercises and pelvic floor therapy, please click on the link below:
Content within askMUSIC is provided by the Urology Care Foundation.
Wherever you are in your prostate cancer journey, joining a support group with men going through or have gone through similar experiences may be a helpful resource to navigate your diagnosis, treatment, and recovery.
Please find prostate cancer support groups below:
Cancer Support Community with University of Michigan Rogel Cancer Center’s Urologic Oncology Program
First Wednesday of the month, 6 PM – 7:30 PM
Program Director Contact:
- Rosie Ingebritson, LMSW
- 734.975.2500
- rosie@cancersupportannarbor.org
Us Too
To find a support group near you, please visit:
https://www.ustoo.org/Support-Group-Near-You
Reel Recovery
“Fly Fishing Retreats for Men Living with Cancer”
State Coordinator/MI Contact:
- Reg Tidball
- 810.877.0199
- regtidball@att.net
Please find caregiver videos of those whose loved ones underwent prostate cancer care, below.
Video 1: What makes an impact in care for prostate cancer patients?
Video 2: How to balance self-care while caring for your loved one with prostate cancer?
Content within askMUSIC is provided by the Urology Care Foundation.