Prostate Cancer Resources for Doctors
Prostate Cancer Apps
Educational Materials
Urology referral patterns and prostate biopsy decision-making have changed in the last 10 years, with biopsy being utilized less frequently in men deemed to be at low risk of prostate cancer. As a result, patients who undergo biopsy today are at greater risk for prostate cancer as compared to patients undergoing biopsy 10 years ago. In light of changing risk levels, it is important to be able to communicate the risk of prostate cancer to patients based on contemporary practice.
We have developed and validated a tool that can help urologists communicate the risk of cancer (no cancer, Gleason 6, Gleason 7 or higher) to patients based on contemporary biopsy practices.
Click below to use the Cancer Risk Tool:
Roadmap for Management of Men With Favorable-Risk Prostate Cancer
In our efforts to continuously improve quality of care for men in Michigan with prostate cancer, the Michigan Urological Surgery Improvement Collaborative (MUSIC) has developed a systematic approach for management of men with favorable-risk, early-stage prostate cancer.
Download the MUSIC Active Surveillance Roadmap
We define men with favorable-risk prostate cancer as patients with early-stage tumors with a Gleason Score of 6 or less, as well as select patients with low-volume Gleason Score 3+4=7 cancer. This information is not intended for men with higher-risk prostate cancer (i.e., high-volume Gleason 3+4=7 or greater).For these men, definitive local treatment is most commonly recommended, but individual discussions will be necessary to determine the best course of action for an individual patient.
After diagnosis, these men should consider Active Surveillance (AS) as one management option.
This roadmap outlines an approach to management of patients with favorable-risk prostate cancer that was developed in the MUSIC collaborative. This approach divides care into two distinct phases that begin at the time of diagnosis:
- Consideration Phase: Steps to take while considering AS
- Surveillance Phase: A roadmap for how to perform AS
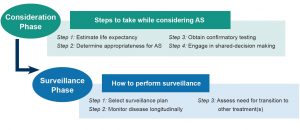
Consideration Phase
The Consideration Phase involves four important steps in determining who is appropriate for Active Surveillance:
Step 1: Estimate life expectancy
Step 2: Determine appropriateness for AS based on MUSIC criteria*
Step 3: Obtain confirmatory testing to further evaluate appropriateness
Step 4: Engage in shared-decision making to make a management decision
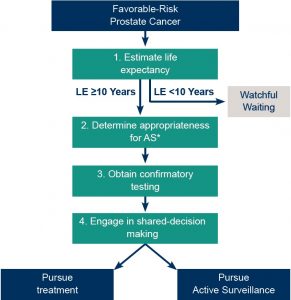
*Some men will choose treatment at this point based on preference or uncertainty around appropriateness for AS.
STEP 1: ESTIMATE LIFE EXPECTANCY
This instrument allows you to determine the average age at which a patient has 10 years of life remaining, accounting for common comorbidities.
If a favorable-risk prostate cancer patient is older than the age listed for their comorbidity group and race, then estimated life expectancy is less than 10 years and Watchful Waiting is often recommended.
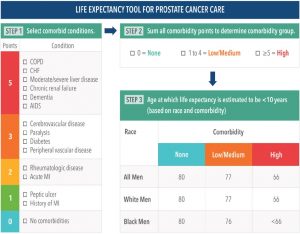
Alternative Tools for Estimating Life Expectancy
1) Social Security actuarial estimate accounting for typical health of prostate cancer patients (Adapted from Kent M, et al. BMC Med 14:25, 2016)
- Age at which average man has 20 years of life remaining: 64-65
- Age at which average man has 10 years of life remaining: 79-80
- If a favorable-risk prostate cancer patient is older than 80, then life expectancy is less than 10 years and Watchful Waiting is often recommended. This age may be younger in men with significant comorbidities as this tool does not account for other medical conditions.
2) Web-based tool evaluating competing risks of death from prostate cancer and other comorbid conditions available at: https://www.mskcc.org/nomograms/prostate
STEP 2: DETERMINE APPROPRIATENESS FOR ACTIVE SURVEILLANCE
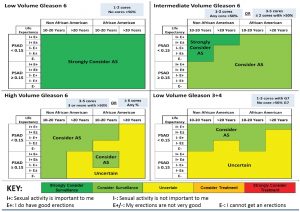
This image summarizes the MUSIC appropriateness panel recommendations for Active Surveillance for 160 different clinical scenarios considered by the panel. Scenarios differed based on Gleason score, tumor volume, PSA density, race, life expectancy, and sexual function/interest.
Directions for use:
- Select a quadrant on this chart based on a patient’s Gleason score and tumor volume.
- Within that quadrant locate the appropriate PSA density and sexual function row.
- Move horizontally across row to the location that matches patient’s life expectancy and race as indicated at the top of table. That location will provide the specific recommendation for a patient meeting all of the criteria.
STEP 3: CONFIRMATORY TESTING
A very important consideration for men diagnosed with favorable-risk prostate cancer is the possibility of underestimating the true grade and/or volume of the tumor. Previous work from MUSIC, and elsewhere, has determined that information available at the time of diagnosis (e.g., PSA, results of diagnostic biopsy, clinical T stage) underestimates the true volume and grade of cancer in 30-50% of patients.
Thus, confirmatory testing is recommended to increase confidence that Active Surveillance is an appropriate form of management. Results from such tests may indicate that definitive local treatment is more appropriate.
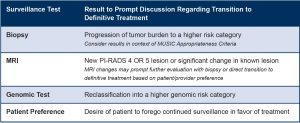
Interpretation of Confirmatory Test Results
One or more of the recommended Confirmatory Tests should be performed within 6 months of diagnosis to increase confidence around appropriate cancer risk-stratification.
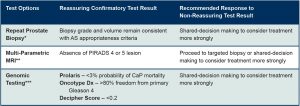
*Should be at least 12 cores, consider anterior sampling or saturation biopsy.
**Obtain at least 6 weeks but no more than 6 months from biopsy. Must involve: 3T magnet, multi-parametric imaging with appropriate sequences (DWI,T2), appropriate radiologic expertise.
***With diagnostic biopsy or repeat biopsy.
STEP 4: ONCE RESULTS OF CONFIRMATORY TESTS ARE AVAILABLE, ENGAGE AGAIN IN SHARED-DECISION MAKING.
At this point, the conversation should reconsider the merits of definitive treatment versus Active Surveillance based on the full set of information from estimation of life expectancy, evaluation of appropriateness, and interpretation of Confirmatory Test results.
Surveillance Phase
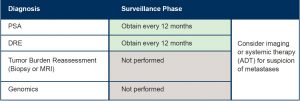
After the Consideration Phase many patients will decide to pursue Active Surveillance. At this point, patients enter the surveillance phase, a period that involves regular follow-up evaluations and testing to monitor for changes in the risk of the cancer. The specific evaluations include PSA testing, clinical examinations, and reassessments of tumor burden via repeat biopsy and MRI imaging.
The goal of this section is to provide a roadmap for how to perform surveillance.
This section outlines two separate surveillance plans (High-intensity and Low-Intensity) that vary with respect to the frequency of follow-up testing. The decision to pursue one pathway or another is based on clinical parameters and patient preferences, guided by the urologist’s opinion and experience. Both surveillance plans are distinctly different from Watchful Waiting, which only involves PSA and clinical examinations.

MUSIC recommends that patients choose between surveillance plans that vary in the frequency of planned follow-up. These plans were modelled on established protocols from centers with extensive experience in Active Surveillance1,2. In the absence of evidence that one plan is clearly superior, the decision for which to pursue should be made between patient and provider after considering risks, benefits and pragmatic aspects of both plans.

*Biopsy should occur at least every 2 years.
+ Genomic testing can be obtained on initial or subsequent biopsy at provider discretion. Consider likelihood of non-reimbursement for repeat genomic testing since this is not yet an established process.
1. High-Intensity Surveillance Plan most consistent with Johns Hopkins protocol — Tosoian JJ, et al., Eur Urol 69:576-81, 2016.
2. Low-Intensity Surveillance Plan most consistent with Toronto protocol — Klotz L, et al., J Clin Oncol 33:272-7, 2015.
Watchful Waiting Plan
Watchful Waiting is typically reserved for men with an estimated life expectancy of less than 10 years.
When to Perform Additional Testing While on Surveillance
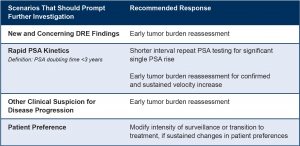
Transitioning to Treatment
If at some point in follow-up a patient’s clinical profile or preferences change, a transition to an alternative management strategy may be warranted.
Transitioning to more aggressive management: Clinical results obtained in follow-up suggesting cancer progression or changing patient preferences may prompt a transition to more aggressive treatment, such as surgery or radiation. In the event that any of the following test results occur, another round of shared-decision making to consider a transition to more definitive treatment is recommended.
Transitioning to Watchful Waiting: Should be considered if new health conditions suggest a patient’s life expectancy drops below 10 years.
If your urology practice utilizes bone scan or CT scan for evaluation of metastatic disease, MUSIC has developed appropriateness criteria for when to consider pursuing one of these tests to evaluate for metastatic disease. These criteria are available for download here:
MUSIC has also developed models for finding an abnormal bone scan or CT scan based on patient characteristics. While the results of these models does not directly factor into the MUSIC appropriateness criteria, they may be useful in communicating the risk of finding metastatic disease to patients.
Click below to access the MUSIC imaging appropriateness criteria and risk models in our app.
Prior to performing a radical prostatectomy, you may consider reviewing the risk of various pathologic outcomes with your patients. These include the following:
- Non-organ-confined disease
- Extraprostatic extension
- Seminal vesicle invasion
- Lymph node invasion
We have developed an app using MUSIC data that predicts the probability of each of these endpoints.