Prostate Cancer: Screening and Diagnosis
The prostate is part of the male reproductive system and its job is to make semen. It is roughly the size of a walnut and sits right below the bladder, surrounding the urethra which is the tube that carries urine from the bladder out through the penis.
About 1 in 9 men will be diagnosed with prostate cancer. Prostate cancer is a type of growth in the prostate cells, that is malignant. The good news is that localized prostate cancer is treatable. Most men who become diagnosed early can live long meaningful lives.
Screening is recommended if you are a man and meet one of the following criteria:
- Between 55-69 years old
- African American and over 40 years old
- Have a family history of prostate cancer
This recommendation is from a guideline issued by the American Urological Association.
For a short video on if prostate cancer screening is right for you, please see below:
Download an informational document on prostate cancer screening
Much of this information was provided by the Urology Care Foundation.
Two ways to help detect prostate cancer early are a prostate-specific antigen (PSA) blood test and digital rectal examination (usually performed by a doctor in the exam room). These tests are not perfect and abnormal results with either test may be due to an enlarged prostate rather than cancer.
What is the prostate-specific antigen, or PSA, blood test?
- PSA is a blood test that detects prostate-specific antigen levels in the blood.
- An elevated PSA might indicate prostate cancer, but other diagnoses such as an enlarged prostate can also cause PSA to to elevated.
- Checking a PSA may help detect prostate cancer early.
For a short video on PSA testing, please see below:
What is a Digital Rectal Exam (DRE)?
- A DRE is when a healthcare provider examines the prostate by placing a lubricated, gloved finger in the rectum after asking the patient to either bend over or lay curled on his side on an exam table. The doctor feels for an abnormal shape or thickness to the prostate.
- This test cannot detect early cancer by itself and should be done with a PSA test.
Much of this information was provided by the Urology Care Foundation.
Prostate cancer is diagnosed by a prostate biopsy. During a prostate biopsy procedure, tiny pieces of tissue are removed from the prostate and examined under a microscope by a pathologist, a doctor who will look at the tissue specifically for cancer cells. The pathologist provides a biopsy report to the doctor which includes useful information, to determine if there is cancer.
For a short video on what you should know about a prostate biopsy, please see below:
 What is the Gleason Score?
What is the Gleason Score?
After a positive biopsy, a Gleason Score is assigned to each tissue sample to decide the risk of the disease and to make an accurate diagnosis. The Gleason score and staging grades how quickly the cells are likely to grow and how likely they are to spread (how aggressive the cancer is)
Prostate cancer can be described as pattern 3, 4, or 5 (with 3 being the less abnormal and 5 being more advanced). The Gleason Score is typically written as Pattern 1 + Pattern 2 = Overall Gleason Score.
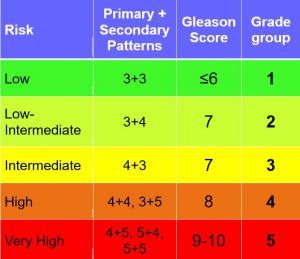
Urologists also use the percent of the tissue that is cancerous to determine prostate cancer risk and help determine appropriate treatment.
Staging
Cancer stage is also measured and describes where the cancer is within the prostate, how extensive it is, and if it has spread to other parts of the body. Staging prostate cancer is done by a DRE, biopsy, and special imaging studies. These staging imaging tests are generally done for men with a Gleason grade 7 or higher and a PSA higher than 10. The system used for tumor staging is called TNM staging which stands for Tumor, Nodes, and Metastasis.
- Tumor (T) Stage: Determined by biopsy or DRE results
- Nodes (N) Stage: Determined by CT Scan
- Metastasis (M) Stage: Determined by Bone Scan
In the early stages, prostate cancer often has no symptoms. When symptoms do occur, they can be like those of an enlarged prostate called benign prostatic hyperplasia (BPH). Prostate cancer can also cause symptoms unrelated to BPH. If you have urinary problems, talk with your healthcare provider about them.
Symptoms of prostate cancer may include the following:
- Dull pain in the lower pelvic area
- Frequent urination and/or trouble urinating (pain, burning, or weak flow)
- Blood in the urine
- Painful ejaculation
- Pain the lower back, hips or upper thighs
- Loss of appetite and/or weight
- Bone pain
Although the cause of prostate cancer is unknown, there are many factors that can increase a man’s risk for the disease. Some of these include:
Age
- Prostate cancer risk increases with age
- Rarely found in men younger than 40
Race/Ethnicity
- Some ethnic groups have a higher risk for prostate cancer
- African American men are more likely to get prostate cancer at an earlier age and have aggressive tumors
- 1 in 6 African American men will get prostate cancer
- Other ethnicities like Hispanic and Asian men are less likely to get prostate cancer
Family History
- Men are 2-3 times more likely to get prostate cancer if their father, brother, or son had prostate cancer
- Risk further increases with the number of relatives diagnosed with prostate cancer
- A relative’s age at diagnosis is also an important factor
Smoking
- Studies have shown that smoking may double your risk for prostate cancer
- Smoking is linked to a higher risk of dying from prostate cancer
- Within 10 years of quitting, a man’s risk of prostate cancer goes down to that of a non-smoker the same age
Geographic Location
- Prostate cancer diagnoses and deaths vary, but higher rates are seen in North America and Northern Europe
- The higher rate of diagnoses may be due to better or more frequent screening procedures, heredity, poor diets, lack of exercise, and environmental exposures
Diet
- Diet may affect prostate cancer risk
- Risk may be higher if patients eat more calories, animal fast, refined sugar, and not enough fruits or vegetables
- Lack of exercise is linked to poor outcomes in patients after treatment


